Dr. Jeff Christiansen Surpasses 300 VetStem Cases

We are happy to announce that another small animal veterinarian has surpassed 300 VetStem Cell Therapy cases! Dr. Jeff Christiansen of Superior Veterinary Surgical Solutions is a board-certified veterinary surgeon based in Florida. He has been providing VetStem services to his patients since 2012. He is one of just two small animal veterinarians who have provided VetStem services to over 300 patients.
Dr. Christiansen integrates regenerative medicine seamlessly into his surgical practice by using it both in conjunction with and in lieu of surgery, depending on the type and severity of injury. While Dr. Christiansen frequently addresses common ailments such as osteoarthritis and cruciate ligament tears, his stem cell expertise extends to a diverse range of injuries and diseases including patella luxation, fractures, spinal conditions, kidney disease, and more. Additionally, Dr. Christiansen has utilized VetStem services for exotic species. In collaboration with a local zoo, he delivered VetStem Cell Therapy to alleviate arthritis in a black bear.
Dr. Christiansen is also an avid user of VetStem’s platelet-rich plasma (PRP) products. While he primarily utilizes PRP for small animal orthopedics and wound healing, Dr. Christiansen has also used PRP to treat various unconventional cases. From treating a fractured limb in a kangaroo to expediting healing after tumor removal in an ostrich, his extensive experience spans a multitude of species and ailments.
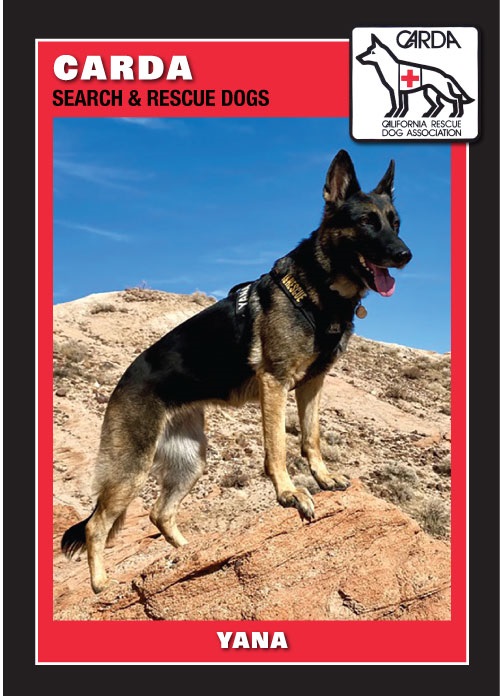
We have shared the stem cell success stories of several of Dr. Christiansen’s patients including Max, a trained companion for a U.S. Army Staff Sergeant and purple heart recipient, who received VetStem Cell Therapy for torn cruciate ligaments. Another one of Dr. Christiansen’s patients, an explosive detection K9, was able to get back to work after receiving VetStem Cell Therapy for hip dysplasia and arthritis. Dr. Christiansen’s dedication to integrating regenerative medicine into his surgical practice has not only transformed the lives of hundreds of furry patients but also underscored the vast potential of VetStem Cell Therapy across a spectrum of species and conditions.